Misinformed fears of HIV infection—and denigrating attitudes and behaviours towards people living with HIV and people at much higher risk of acquiring infection—have been features of the HIV epidemic for decades. HIV-related stigma and discrimination continues to do harm by aggravating the HIV and other health threats that people face, and by obstructing people from acquiring the information and making use of the services they need to protect their health.
Legal systems in many countries are failing to protect the people that HIV responses are trying to reach. Criminalization of same-sex sexual relationships, sex work and drug use give license to discrimination, harassment and violence, isolating key populations and hindering them from accessing vital services. Overly broad criminalization of HIV non-disclosure, exposure or transmission also deters people from seeking to know their HIV status or from accessing HIV services.
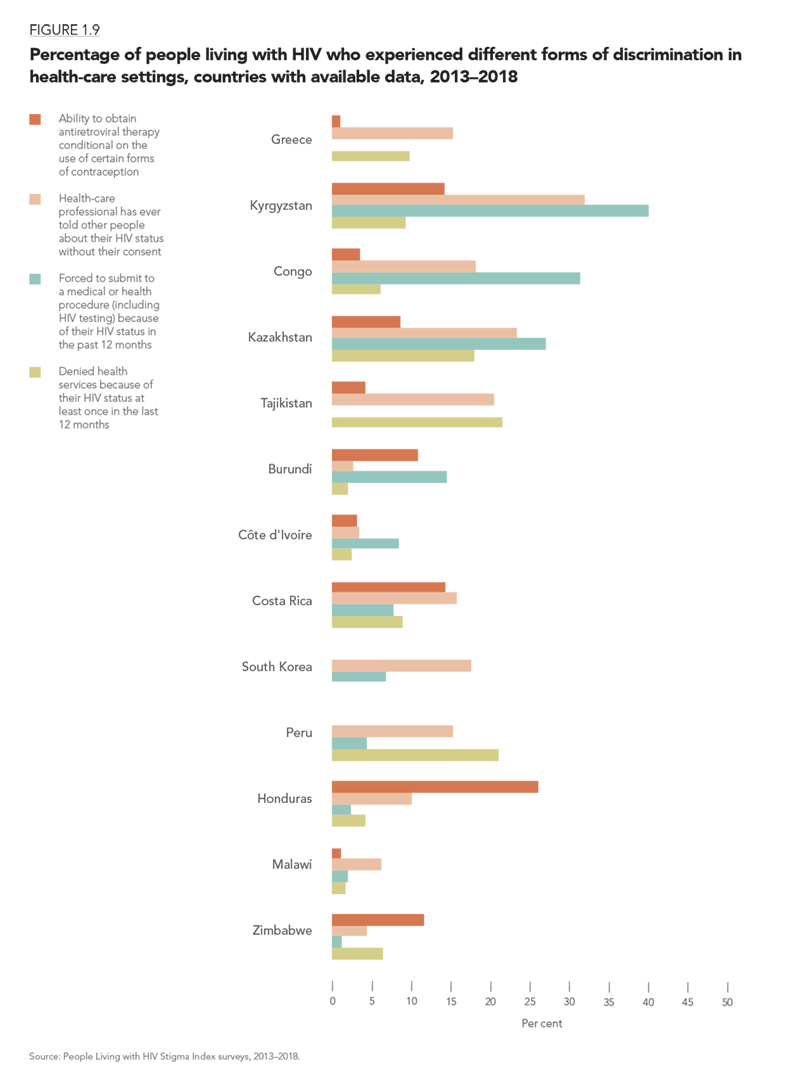
Levels of HIV-related stigma and discrimination are currently tracked through population-based surveys, which reveal discriminatory attitudes within the general population, and through surveys that ask people living with HIV and members of key populations whether they have experienced stigma and discrimination within the previous 12 months. Efforts are ongoing to strengthen the monitoring of stigma and discrimination as countries and communities aim to reach the goal of zero discrimination.
The most recent data from population-based surveys show that while discriminatory attitudes towards people living with HIV—measured by whether a person would buy fresh vegetables from a shopkeeper living with HIV—are declining consistently in some countries, they are rebounding in others. In eastern and southern Africa, for instance, discriminatory attitudes have been reduced in some countries to historically low levels. Elsewhere, however, disconcertingly large proportions of adults continue to hold discriminatory attitudes towards people living with HIV. In 25 of 36 countries with recent data on a composite indicator that includes two types of discriminatory attitudes, more than 50% of people aged 15 to 49 years reported having discriminatory attitudes towards people living with HIV.
Surveys of people living with HIV confirm
that stigma and discrimination at health-care facilities—in the shape of denial of care, dismissive attitudes, coerced procedures or breach of confidentiality—remain disturbingly common. This discourages people living with HIV from knowing their HIV status and seeking care. Such poor treatment from health-care providers also makes it more difficult for people living with HIV to adhere successfully to treatment, achieve the sustainable viral load required for their own health and reduce the risk of transmitting HIV to others.
Across 13 countries with available data, the percentage of people living with HIV who reported being denied health services at least once in the previous 12 months because of their HIV status ranged from 1.7% in Malawi to as high as 21% in Peru and Tajikistan. Coerced medical or health procedures remain common, as do breaches of confidentiality by health-care professionals (reported by at least 15% of people in eight of 13 countries with available data). Significant proportions of people living with HIV also reported that their ability to obtain antiretroviral therapy was conditional on them using certain forms of contraception.