A combination approach to HIV prevention that includes behavioural, biomedical and structural approaches and is tailored to those in greatest need can lead to steep reductions in HIV infections. The launch of the Global HIV Prevention Coalition in 2017 sparked renewed focus among participating countries towards achieving global prevention targets. However, major gaps remain.
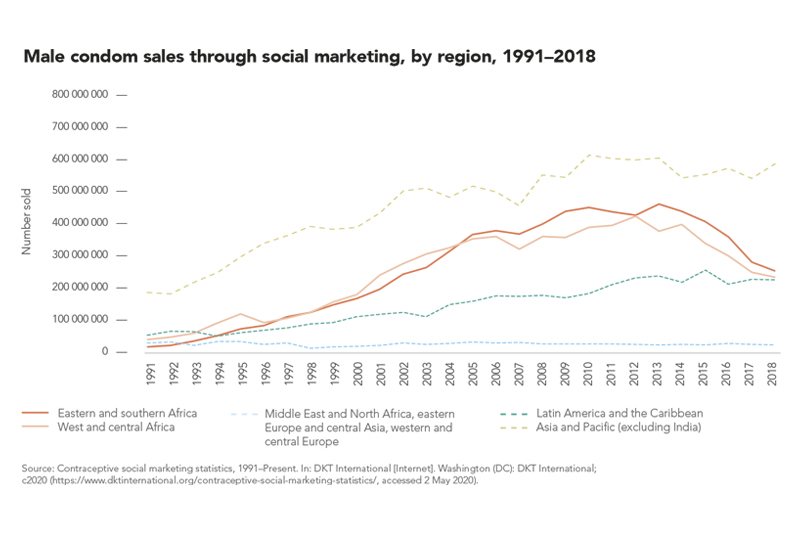
The defunding of condom social marketing programmes and decline in sales of socially marketed condom in sub-Saharan Africa is emblematic of a decreased focus on condom demand generation, reduced emphasis on condoms in family planning services and weak stewardship of condom programmes since 2010, leaving the world far off the 90% target for condom use. A new generation of sexually active young people has not been exposed to the intense condom promotion that was in place a decade ago. Condom use at last higher risk sex reported by young women (aged 15 to 24 years) declined in five countries in western and central Africa and three countries in eastern and southern Africa. Condom use at higher risk sex among men (aged 15 to 49 years) also declined in five out of nine countries (compared to the previous survey).
Key population access to combination HIV prevention options varies greatly among countries, and it remains insufficient globally. In six of 13 countries that have conducted surveys since 2016 and reported those data to UNAIDS, less than half of transgender women stated that they were able to access at least two HIV prevention services in the past three months. The same is true for female sex workers in 16 of 30 reporting countries, for gay men and other men who have sex with men in 26 of 38 reporting countries and for men who inject drugs in 10 of 14 reporting countries.
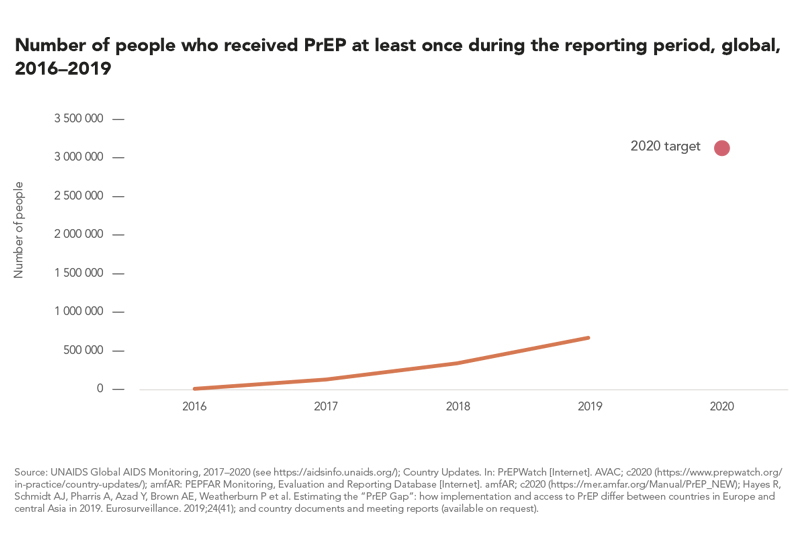
The number of people reported to have received PrEP at least once in the previous year has increased dramatically in recent years, from fewer than 2000 in 2016 to more than 590 000 in 2019. In several cities in North America, Europe and Australia where PrEP is widely available, this relatively new prevention tool has contributed to steep reductions in HIV infections among gay men and other men who have sex with men. Global coverage, however, is still far short of the 2020 target of 3 million receiving PrEP (see Chapter 5 for additional analysis).
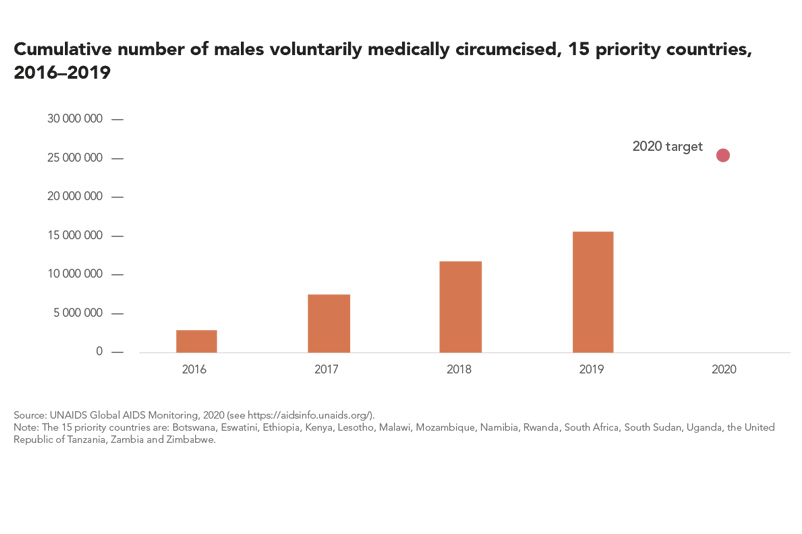
Voluntary medical male circumcision (VMMC) provides lifelong partial protection against female-to-male HIV transmission, reducing heterosexual male vulnerability to HIV infection by approximately 60%. VMMC can also act as an entry point for providing men and boys with broader health packages to improve their health outcomes. When combined with high levels of treatment coverage and viral suppression, evidence shows that the impact of VMMC is particularly significant.
By the end of 2019, more than 15 million men and boys across 15 priority countries had been voluntarily and medically circumcised since the beginning of 2016, 4.2 million of them in 2019 alone. Among 12 priority countries that reported age-disaggregated data, about 40% of those who underwent VMMC were between the ages of 10 and 14.
Among the priority countries, the United Republic of Tanzania performed the most VMMCs (nearly 800 000) in 2019. Annual circumcisions in the 15 priority countries have remained relatively stable since 2017, falling short of the annual amounts needed to reach the 2020 target of 25 million additional circumcisions since the beginning of 2016.